Colorectal or Colon Cancer
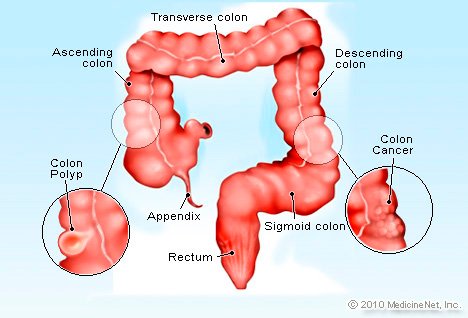
As the name indicates, Colorectal or colon cancer starts in the colon or rectum. These organs constitute the lower portion of the human digestive system. A colon is also referred to as the large intestine, and the rectum is situated at the end of the colon.
According to research, nearly 1 out of 22 men and 1 out of 24 women suffer from colorectal cancer.
To define the criticalness of cancer, stages are defined for it ranging from Stage 1 which is the earliest stage and less critical to Stage 4 which is the most advanced stage. Let’s know each of them in detail:
1st Stage Colon cancer: In this, cancer penetrates the lining of the colon or rectum and is limited to only this organ and has not spread to walls of it.
2nd Stage Colon cancer: Cancer spread to the colon walls but don’t affect nearby tissues and lymph nodes.
3rd Stage Colon cancer: In this stage, cancer spreads to the regional lymph nodes and may involve nearby organs but not to other body parts.
4th Stage Colon cancer: Cancer gets spread to the non-regional lymph nodes and distant organs of the body.
Symptoms
You may not experience the symptoms of colorectal cancer in the starting stage. But however, if you experience the symptoms may include:
- Long-standing diarrhea or constipation.
- Stool color will get changed along with the consistency.
- Blood in stool .
- Abdominal cramps and pain.
- Excessive gas.
In stage 4 Colon cancer:
When cancer gets spread to the other parts of the body, then the possible symptoms are:
- Jaundice
- Swelling
- Difficulty in breathing
- Headaches
- Blurred vision
- Fractures in bone
Causes:
There are many risk factors that increase the risk of developing colorectal cancer. These includes:
Precancerous growths: The abnormal cells accumulate in the colon lining form polyps. Polyps are small and not harmful. These can be removed by surgery, however, if not removed then they can become cancerous.
Genetic Factors:
When a gene mutation passes from the parents to the child, it can probably result in colon cancer. Some genetic syndromes are also responsible for colorectal cancer especially in younger age.
Avoidable risk factors of Colorectal Cancer:
The factors which are avoidable means you can reduce the risk by changing the habits. These include:
- Obesity
- Smoking habit
- Alcohol consumption
- Lethargic Lifestyle
- High intake of fatty food
Screening for colorectal cancer:
Screening can detect colorectal cancer at an earlier stage so that cancer can be cured.
American Cancer Society Guideline for Colorectal Cancer Screening
People at average risk* of colorectal cancer start regular screening at age 45.
People who are in good health and with a life expectancy of more than 10 years should continue regular colorectal cancer screening through the age of 75.
For people ages 76 through 85, the decision to be screened should be based on a person’s preferences, life expectancy, overall health, and prior screening history.
People over 85 should no longer get colorectal cancer screening.
*For screening, people are considered to be at average risk if they do not have:
- A personal history of colorectal cancer or certain types of polyps
- A family history of colorectal cancer
- A personal history of inflammatory bowel disease (ulcerative colitis or Crohn’s disease)
- A confirmed or suspected hereditary colorectal cancer syndrome, such as familial adenomatous polyposis (FAP) or Lynch syndrome (hereditary non-polyposis colon cancer or HNPCC)
- A personal history of getting radiation to the abdomen (belly) or pelvic area to treat a prior cancer
People at increased or high risk of colorectal cancer might need to start colorectal cancer screening before age 45, be screened more often, and/or get specific tests. This includes people with:
- A strong family history of colorectal cancer or certain types of polyps (see Colorectal Cancer Risk Factors)
- A personal history of colorectal cancer or certain types of polyps
- A personal history of inflammatory bowel disease (ulcerative colitis or Crohn’s disease)
- A known family history of a hereditary colorectal cancer syndromes such as familial adenomatous polyposis (FAP) or Lynch syndrome (also known as hereditary non-polyposis colon cancer or HNPCC)
Test options for colorectal cancer screening
Several test options are available for colorectal cancer screening:
Stool-based tests
- Highly sensitive fecal immunochemical test (FIT) every year
- Highly sensitive guaiac-based fecal occult blood test (gFOBT) every year
- Multi-targeted stool DNA test (MT-sDNA) every 3 years
Visual (structural) exams of the colon and rectum
Colonoscopy every 10 years
- CT colonography (virtual colonoscopy) every 5 years
- Flexible sigmoidoscopy (FSIG) every 5 years
Treatment:
Colon Cancer:
- Stage 1 Colon cancer: surgery only
- Stage 2 Colon cancer: surgery only and sometimes chemotherapy is also given after surgery
- Stage 3 Colon cancer: surgery followed by Chemotherapy
- Stage 4 Colon cancer: Chemotherapy + Targeted therapy, Immunotherapy. sometimes surgery is also done
Rectal Cancer:
- Stage 1 Rectal Cancer: surgery only
- Stage 2 Rectal Cancer: surgery only and sometimes chemotherapy is also given after surgery
- Stage 3 Rectal Cancer: Radiotherapy + surgery + Chemotherapy
- Stage 4 Rectal Cancer: Chemotherapy +Targeted therapy, Immunotherapy. sometimes surgery is also done