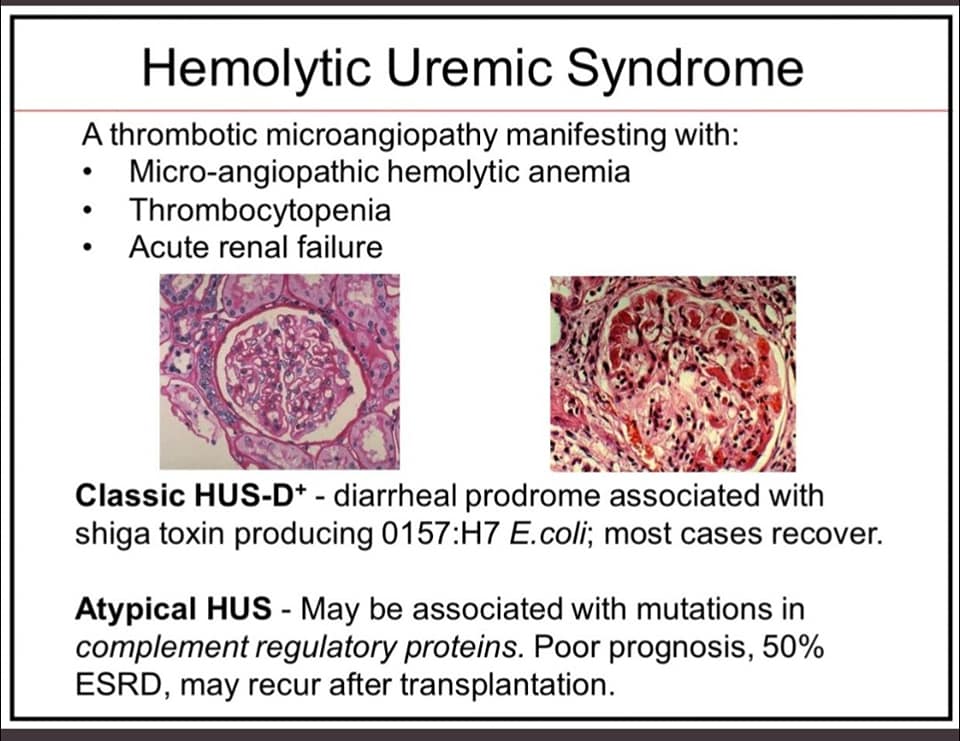
AHUS Is A Disease Of Excessive Activation Of The Alternative Complement Pathway (ACP)
11 Mar, 2021
Dr. Rajesh Bollam
Recent Posts

Bone Marrow Transplantation in children
Aug 27, 2024
Dr. Rajesh Bollam

All you need to know about Childhood Cancers
Aug 26, 2024
Dr. Rajesh Bollam

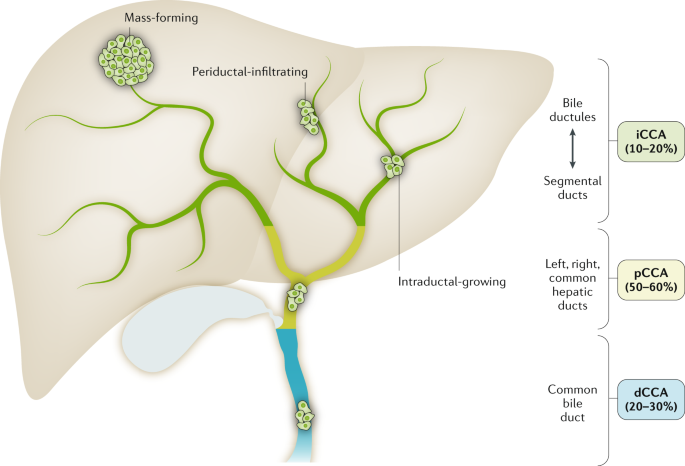
Signs of Liver Cancer
May 30, 2024
Dr. Rajesh Bollam
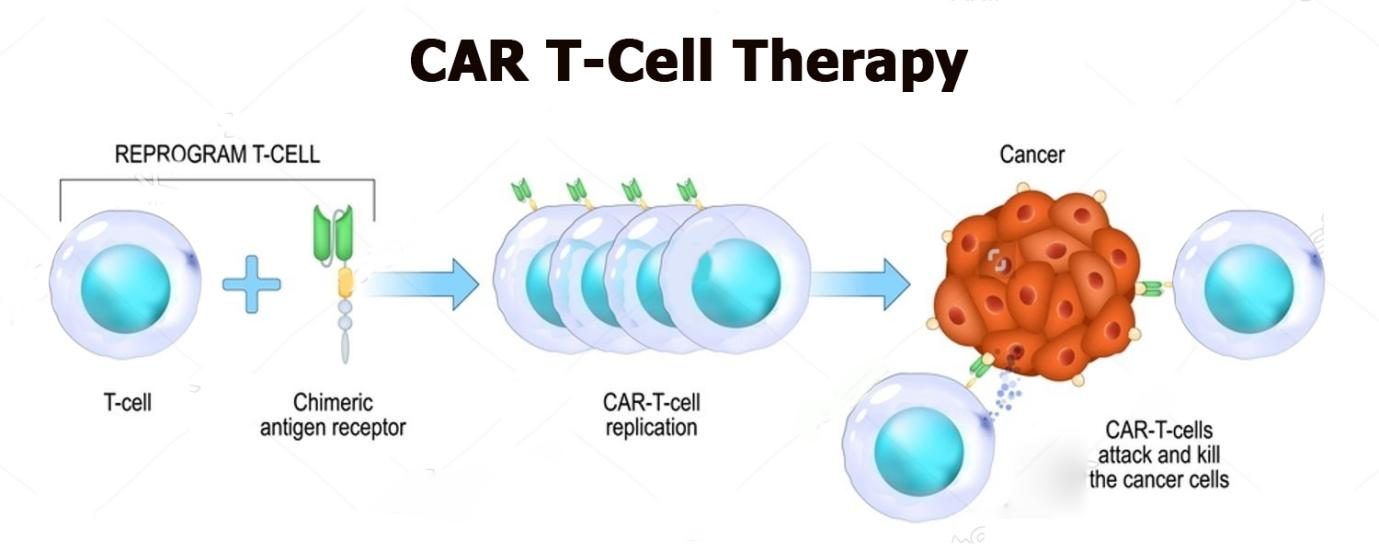
CAR T-cell therapy
Mar 01, 2024
Dr. Rajesh Bollam

Mediastinal tumors
Jun 03, 2022
Dr. Rajesh Bollam
.jpg)
Blood Cancer Journal
Apr 29, 2022
Dr. Rajesh Bollam
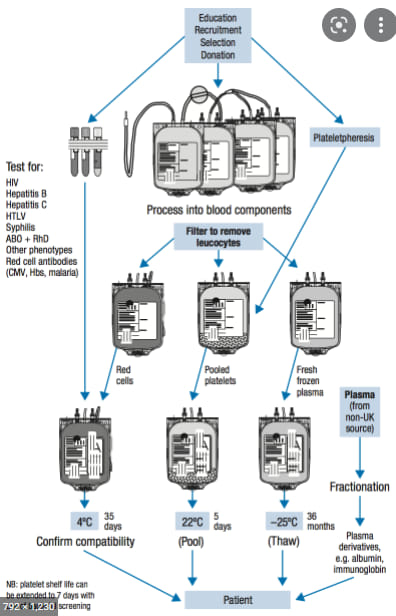
Transfusion medicine for RBCs
Apr 18, 2022
Dr. Rajesh Bollam
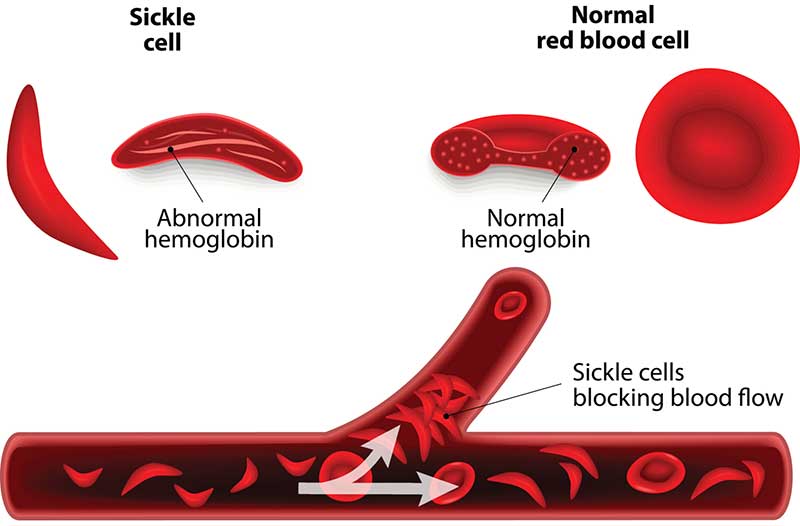
Sickle Cell Anemia
Apr 15, 2022
Dr. Rajesh Bollam
What’s new in cancer immunotherapy?
Nov 30, 2021
Dr. Rajesh Bollam

What is immunotherapy?
Nov 30, 2021
Dr. Rajesh Bollam
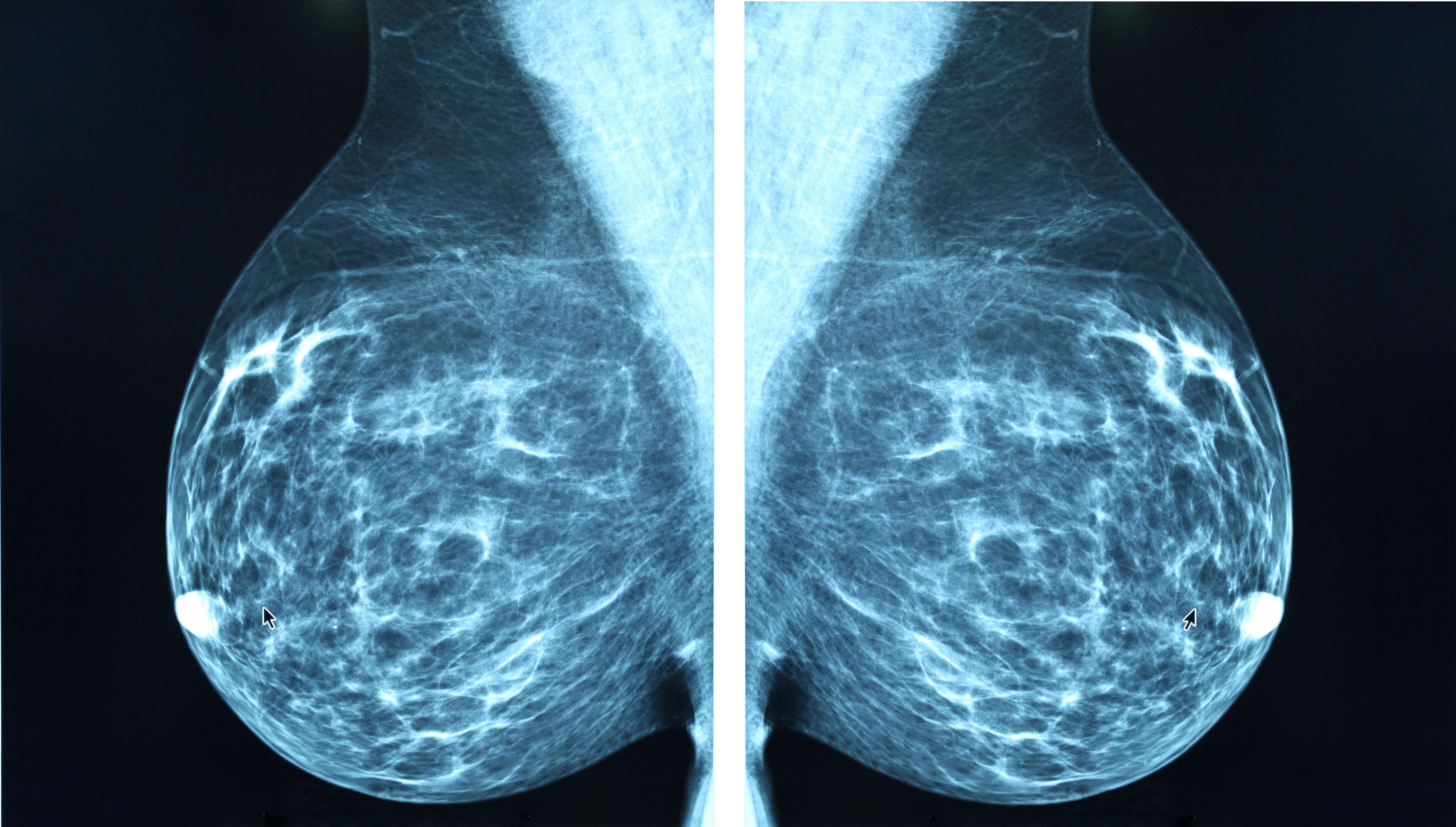
What causes breast cancer?
Nov 30, 2021
Dr. Rajesh Bollam

Who gets breast cancer?
Nov 30, 2021
Dr. Rajesh Bollam
Breast cancer symptoms
Nov 30, 2021
Dr. Rajesh Bollam
.jpg)
Types of breast cancer
Nov 30, 2021
Dr. Rajesh Bollam
Types of invasive breast cancers
Nov 30, 2021
Dr. Rajesh Bollam
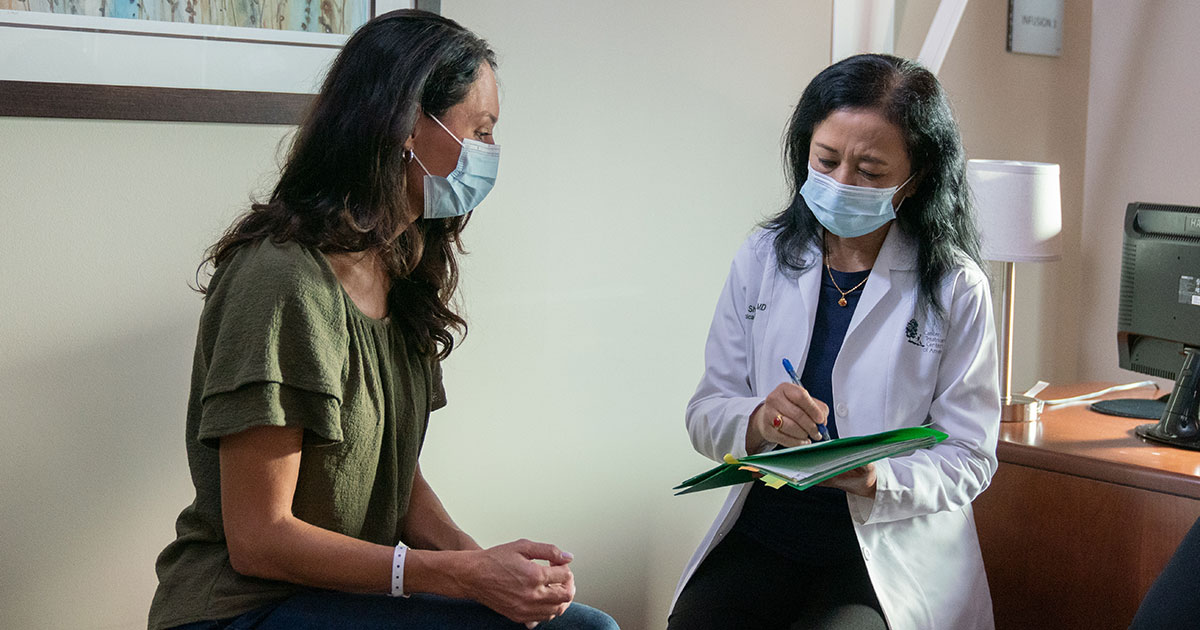
Breast cancer treatment plan
Nov 30, 2021
Dr. Rajesh Bollam
How to prevent cervical cancer
Nov 22, 2021
Dr. Rajesh Bollam
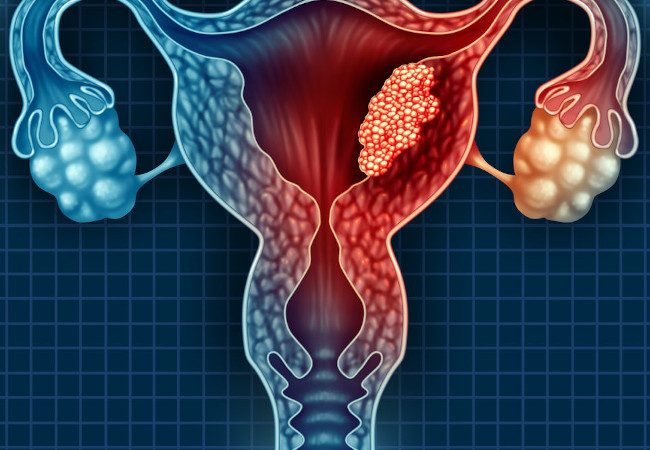
What is cervical cancer?
Nov 22, 2021
Dr. Rajesh Bollam

Are there tests for early detection?
Nov 22, 2021
Dr. Rajesh Bollam

Breast cancer risk factors
Nov 22, 2021
Dr. Rajesh Bollam
Staging and Treatment for oral cancer
Nov 22, 2021
Dr. Rajesh Bollam

How to prevent oral cancer
Nov 22, 2021
Dr. Rajesh Bollam

Risk factors of oral cancer
Nov 22, 2021
Dr. Rajesh Bollam

What is oral cancer?
Nov 22, 2021
Dr. Rajesh Bollam
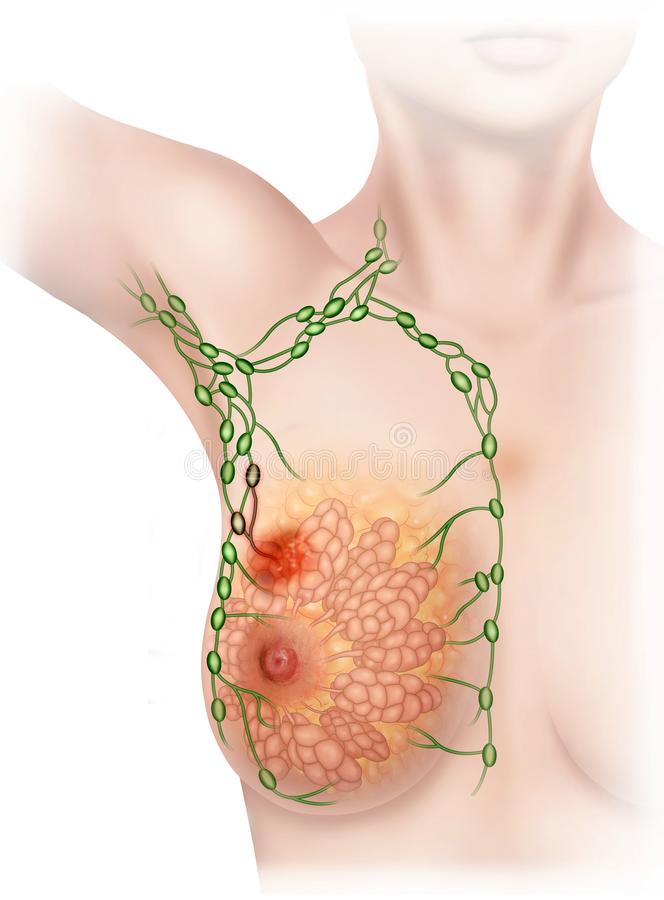
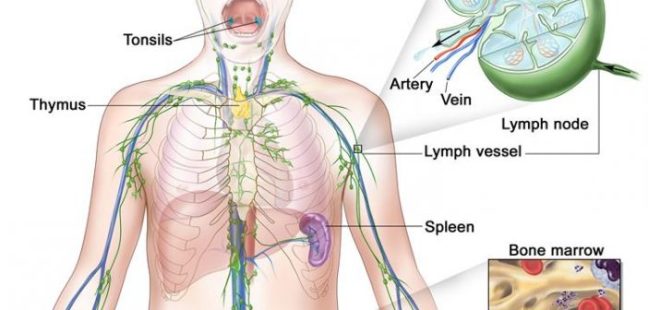
The Lymph System of the Breast
Nov 22, 2021
Dr. Rajesh Bollam
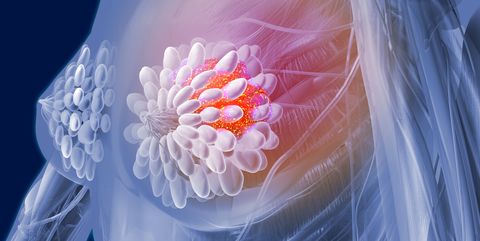
What Is Breast Cancer?
Nov 22, 2021
Dr. Rajesh Bollam
.jpeg)
Kidney Cancer: Myths & Reality
Nov 12, 2021
Dr. Rajesh Bollam
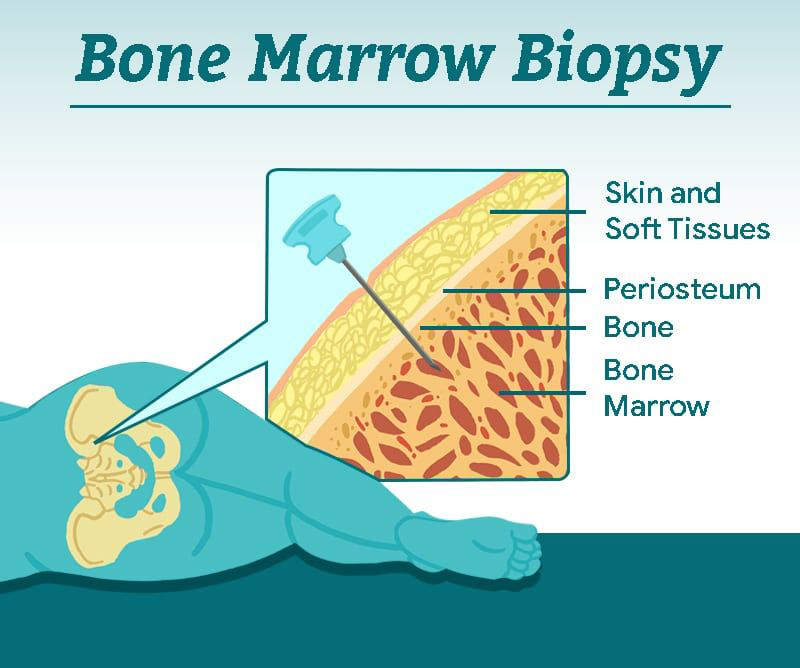
Bone marrow biopsy
Sep 29, 2021
Dr. Rajesh Bollam
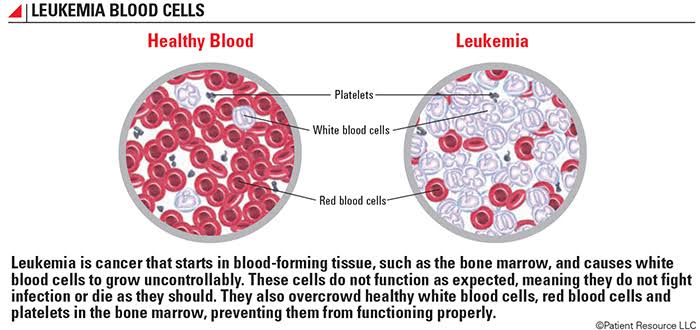
Leukemia
May 28, 2021
Dr. Rajesh Bollam
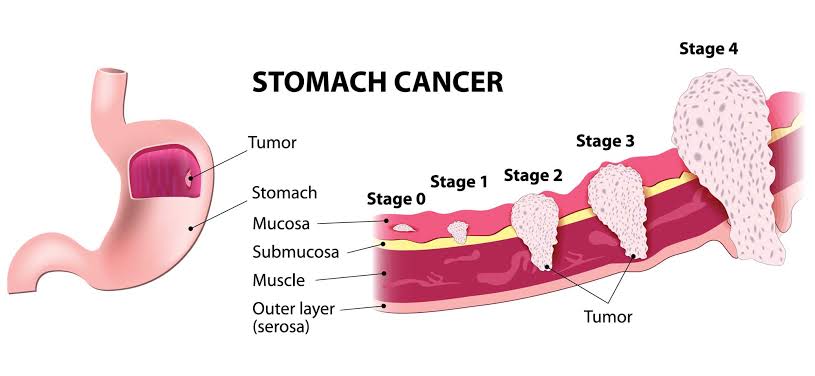
Stomach Cancer
May 28, 2021
Dr. Rajesh Bollam
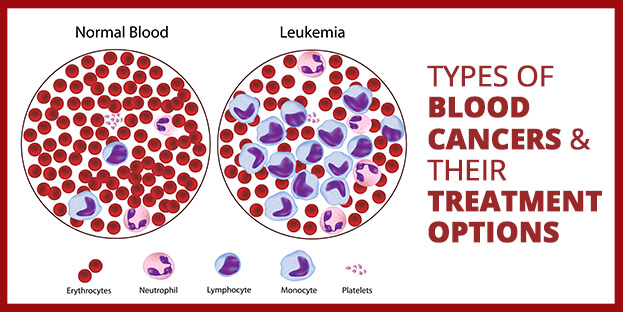
Blood Cancer – Types and Treatment
May 21, 2021
Dr. Rajesh Bollam
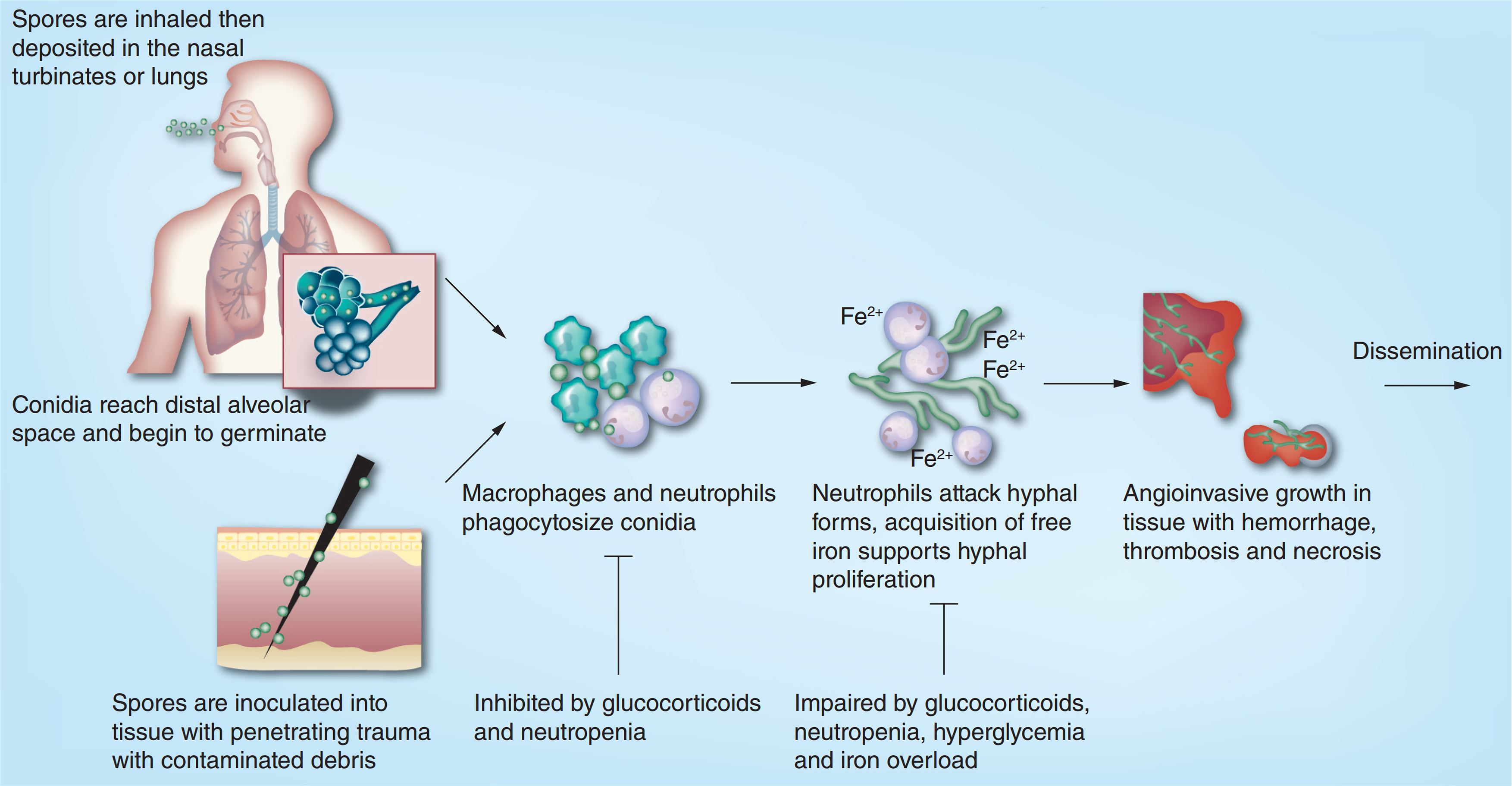
Reasons for mucormycosis in Covid-19
May 21, 2021
Dr. Rajesh Bollam
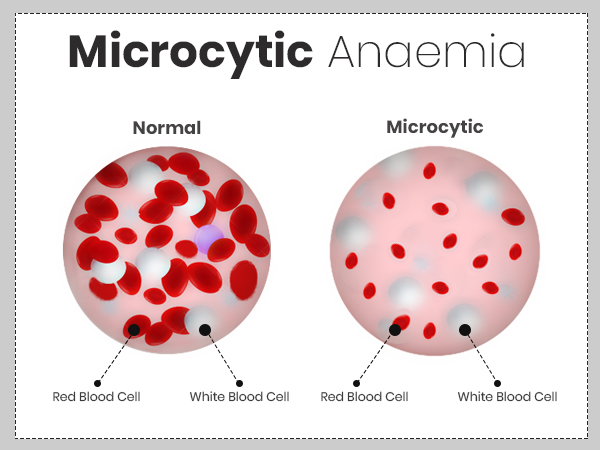
Microcytic and Hypochromic anemia is one of the common scenario we encounter in Clinics
May 21, 2021
Dr. Rajesh Bollam
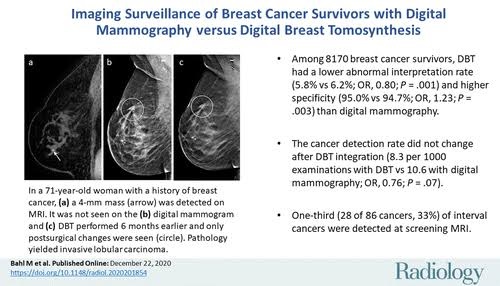
Updated Recommendations for Breast Cancer Surveillance in Young Female Cancer Survivors
May 21, 2021
Dr. Rajesh Bollam
vs
May 14, 2021
Dr. Rajesh Bollam
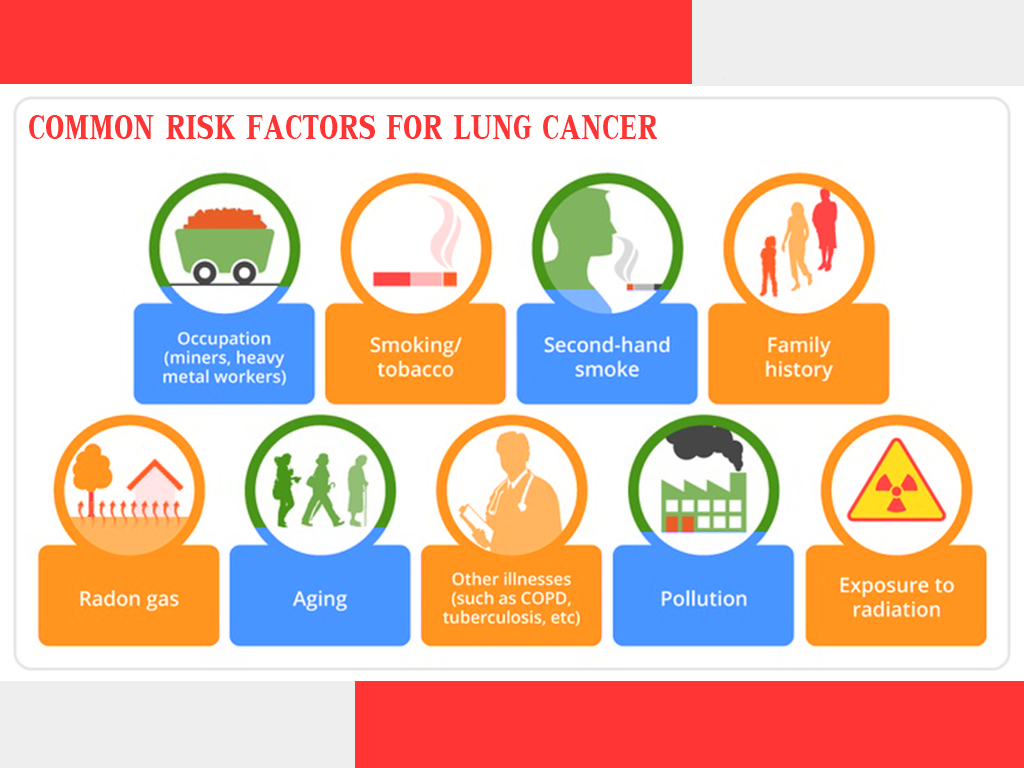
Risk Factors of Lung Cancer
Apr 06, 2021
Dr. Rajesh Bollam
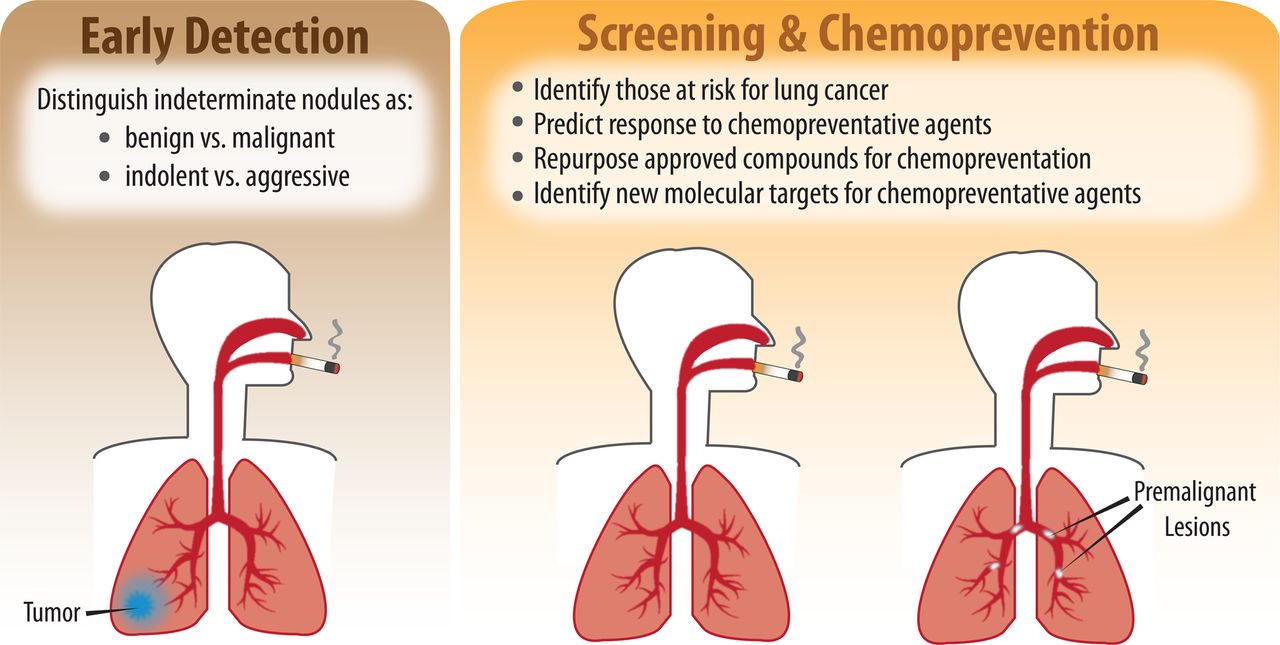
Diagnosing lung cancer
Apr 06, 2021
Dr. Rajesh Bollam
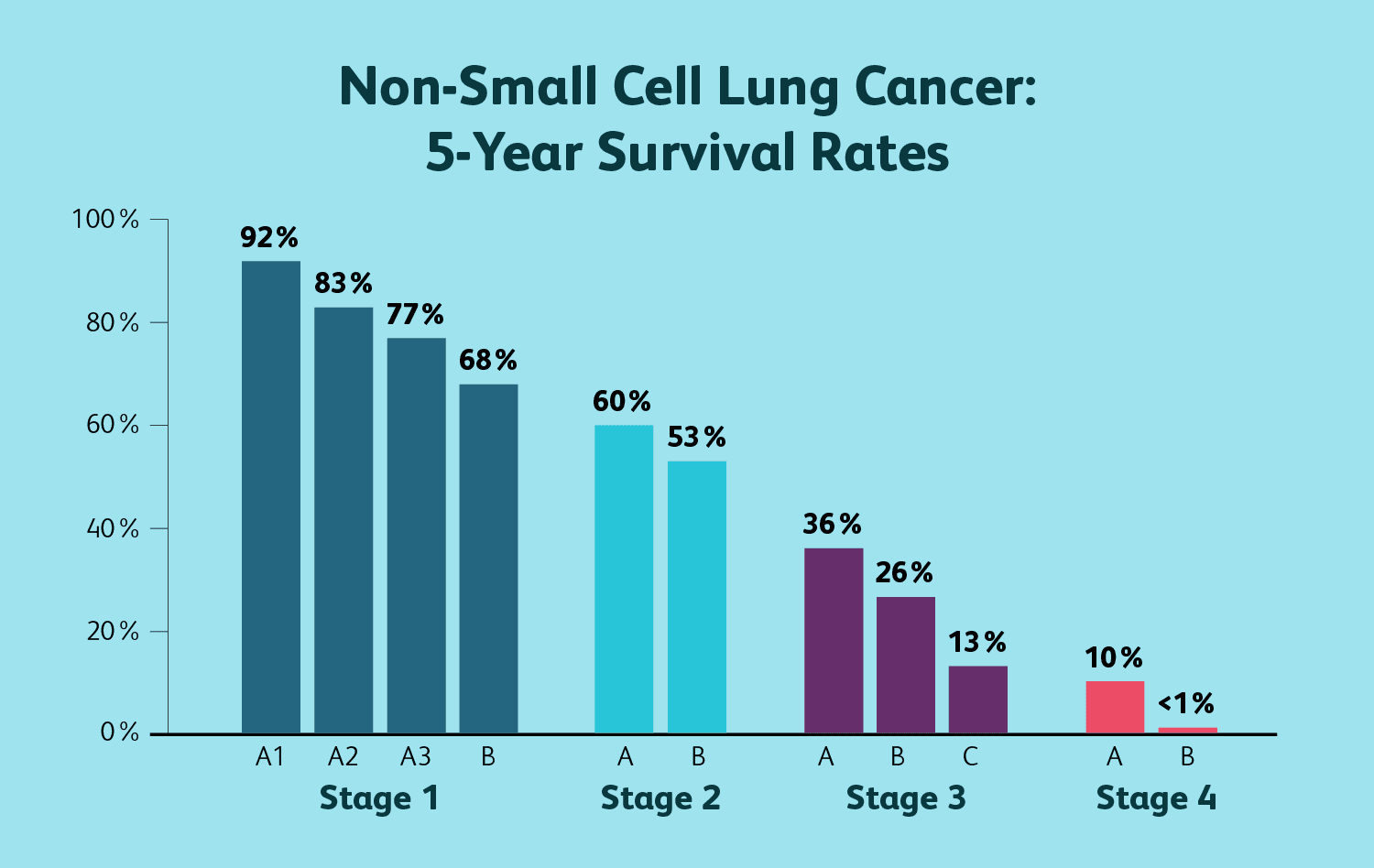
Lung cancer and life expectancy
Apr 06, 2021
Dr. Rajesh Bollam

Home remedies for lung cancer symptoms
Apr 06, 2021
Dr. Rajesh Bollam
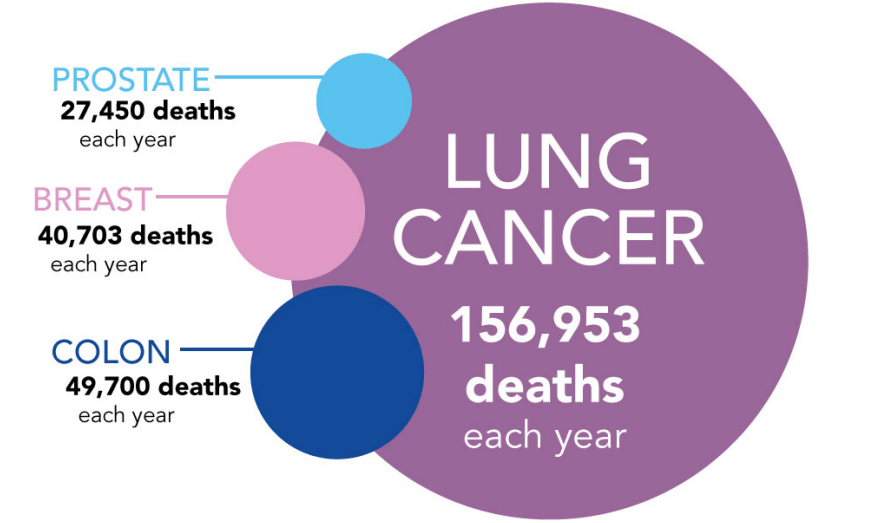
Facts and statistics about lung cancer
Apr 06, 2021
Dr. Rajesh Bollam

Diet recommendations for people with lung cancer
Apr 06, 2021
Dr. Rajesh Bollam
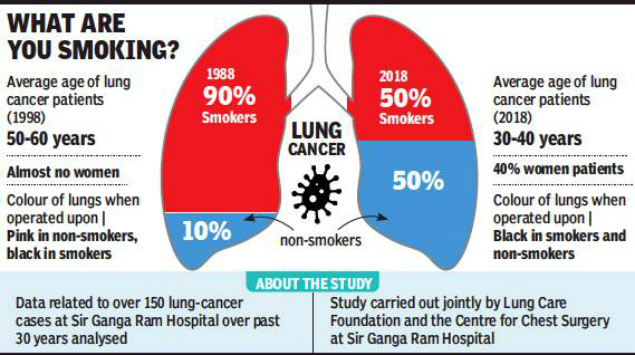
Lung cancer and smoking
Apr 06, 2021
Dr. Rajesh Bollam
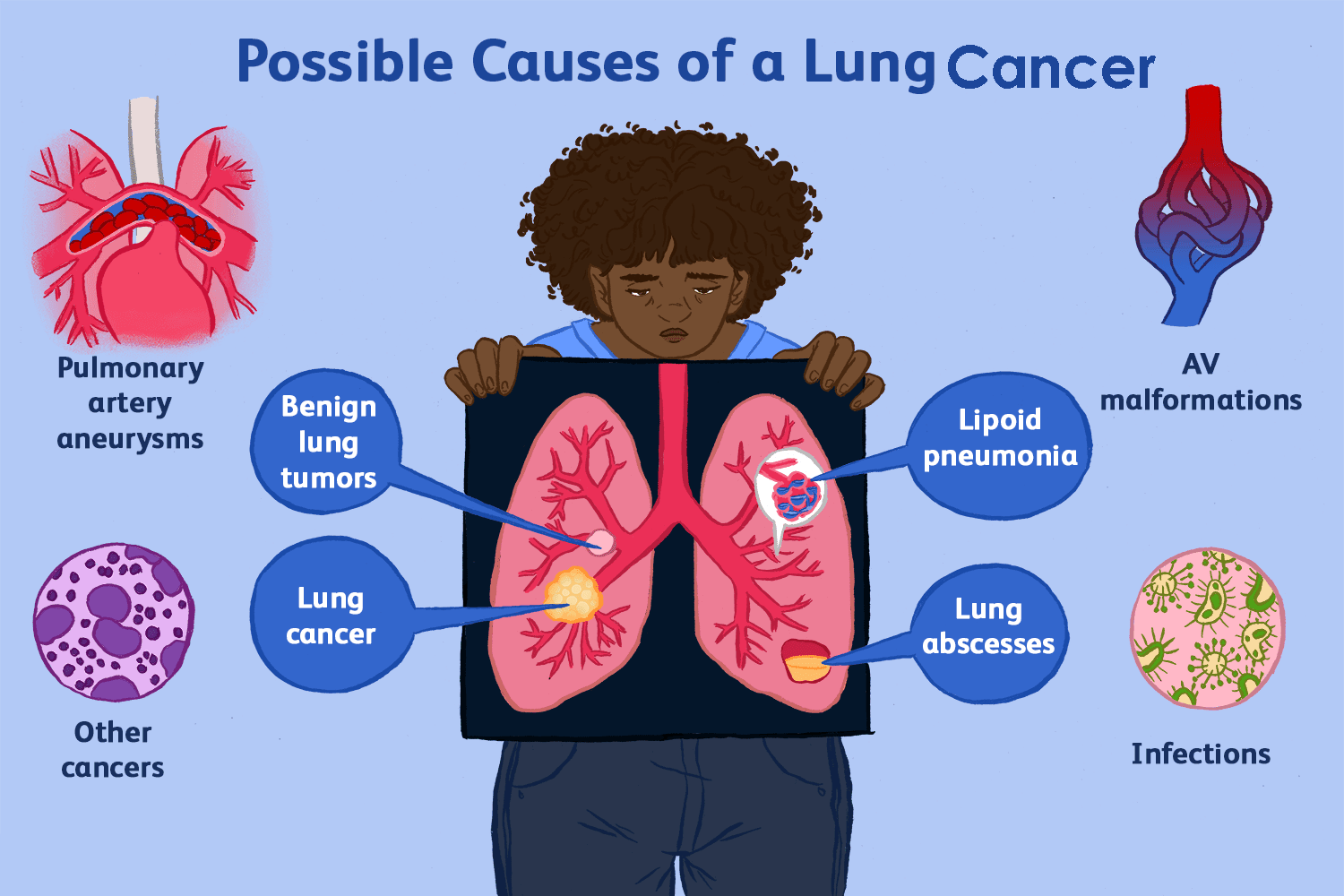
Causes of Lung Cancer
Apr 06, 2021
Dr. Rajesh Bollam
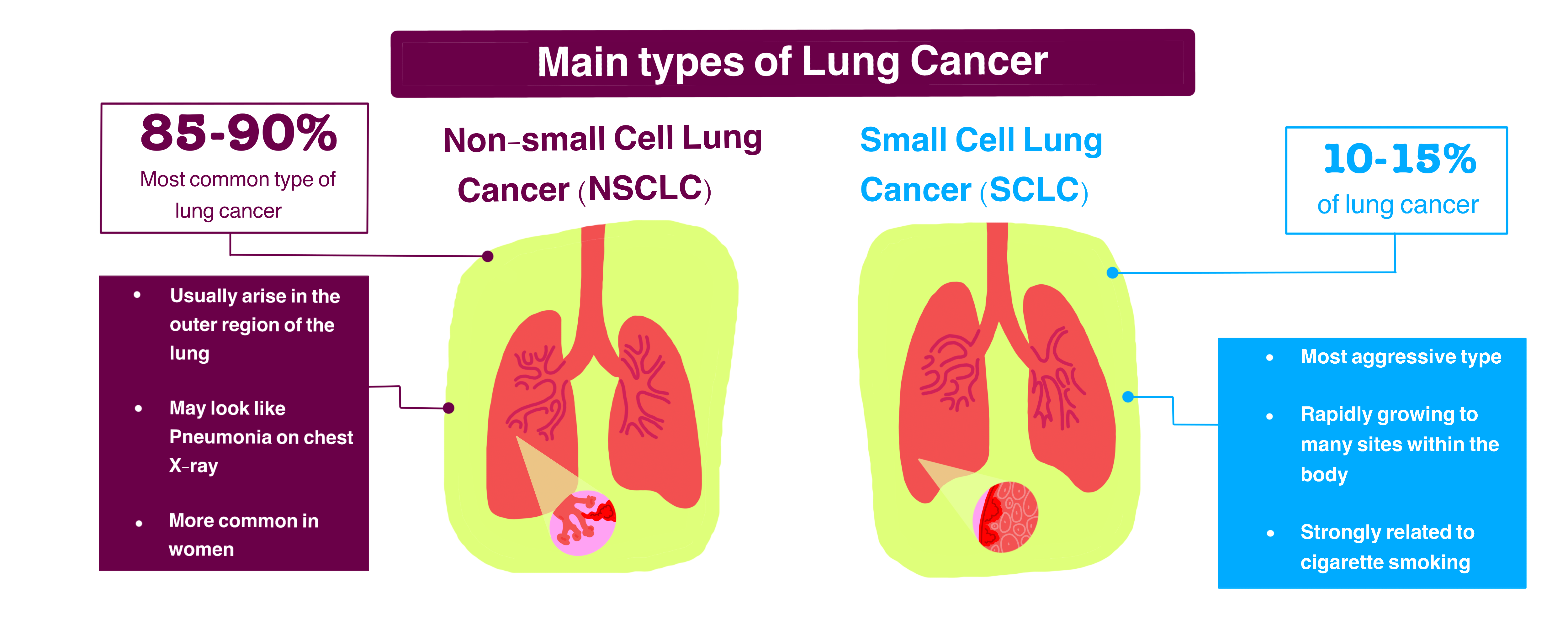
Different Types of Lung Cancer
Apr 06, 2021
Dr. Rajesh Bollam
Lung Cancer and its types
Apr 06, 2021
Dr. Rajesh Bollam
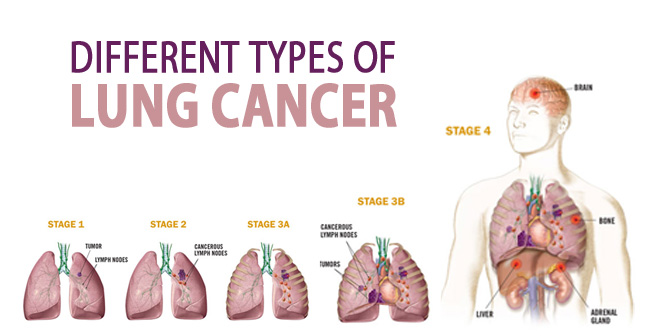
Stages of LUNG CANCER
Apr 06, 2021
Dr. Rajesh Bollam
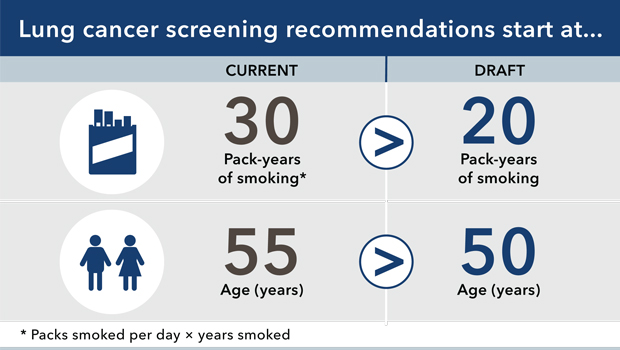
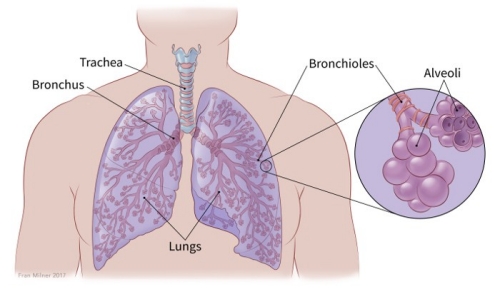
Lung Cancer and Lung Cancer Screening
Apr 06, 2021
Dr. Rajesh Bollam
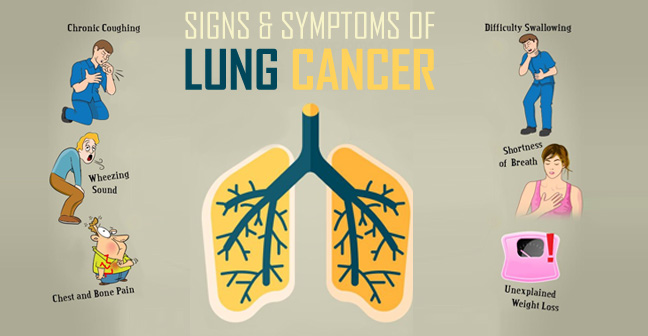
What are the symptoms of lung cancer
Apr 06, 2021
Dr. Rajesh Bollam
Lung cancer occurs when cells divide in the lungs uncontrollably.
Apr 06, 2021
Dr. Rajesh Bollam
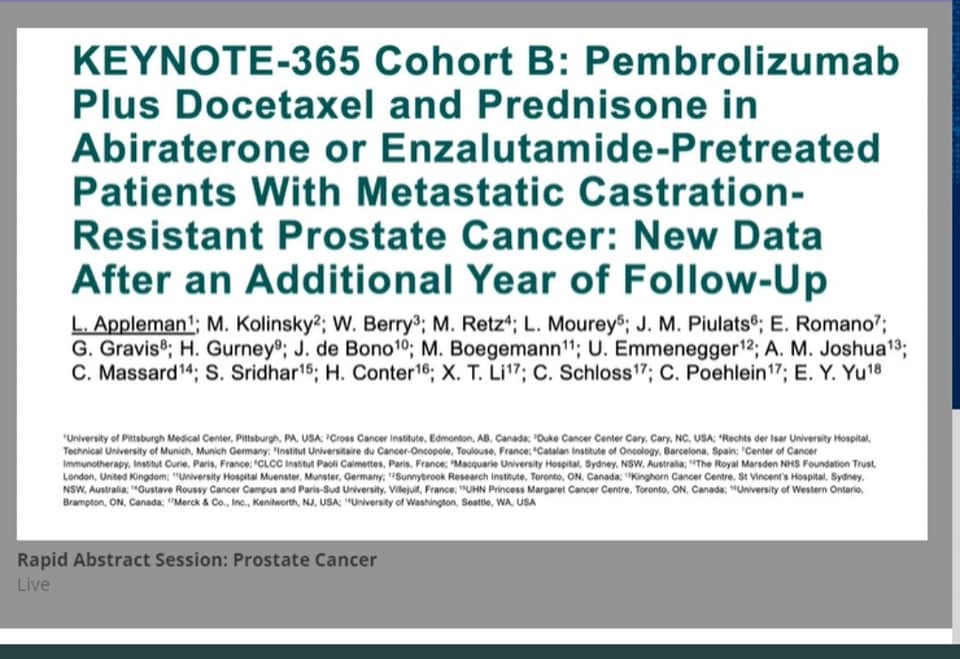
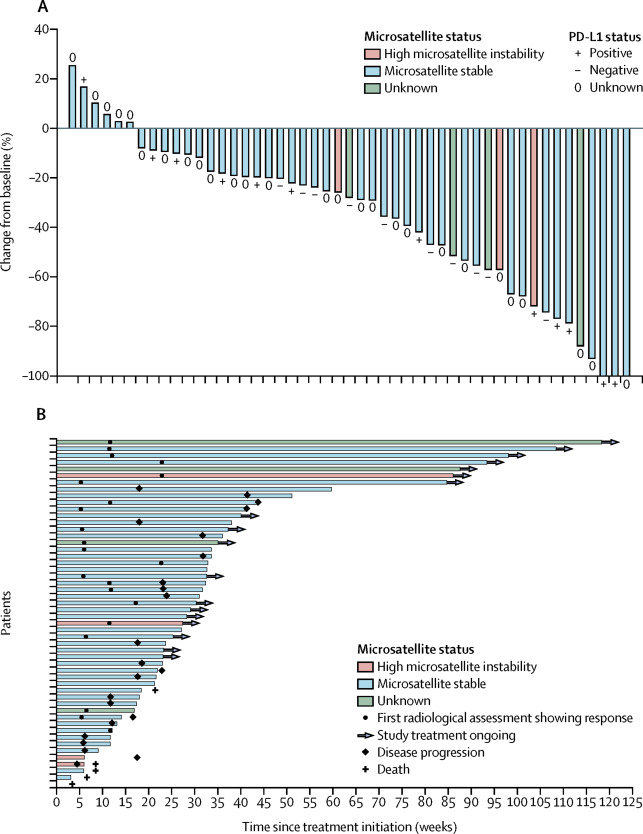
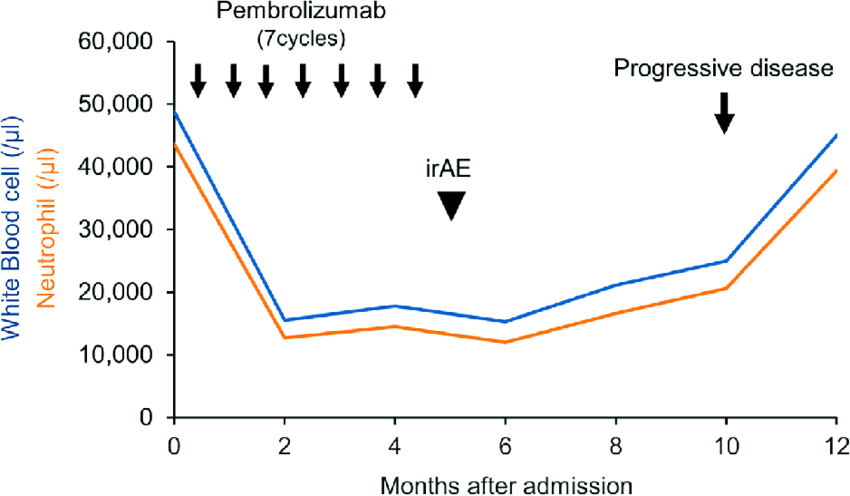
KEYNOTE-365
Mar 12, 2021
Dr. Rajesh Bollam
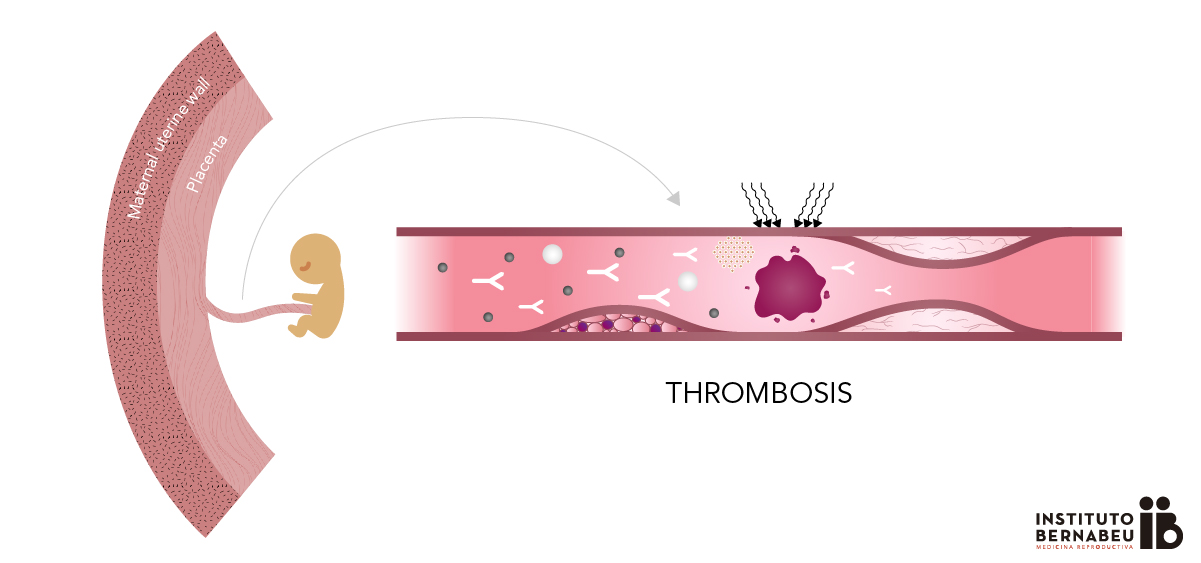
Antiphospholipid syndrome in Pregnancy
Mar 12, 2021
Dr. Rajesh Bollam
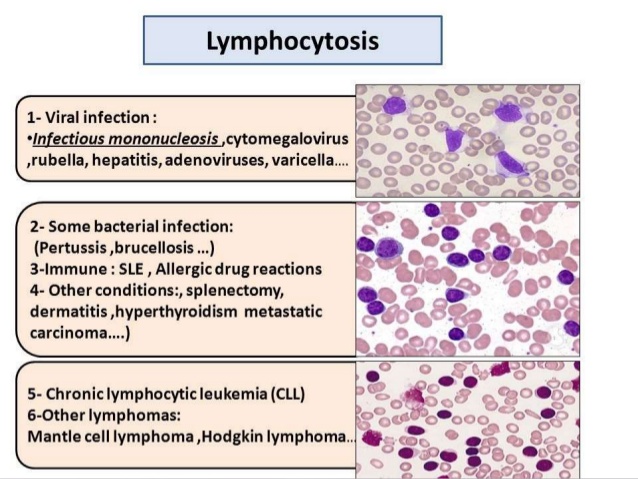
Leucocytosis
Mar 12, 2021
Dr. Rajesh Bollam
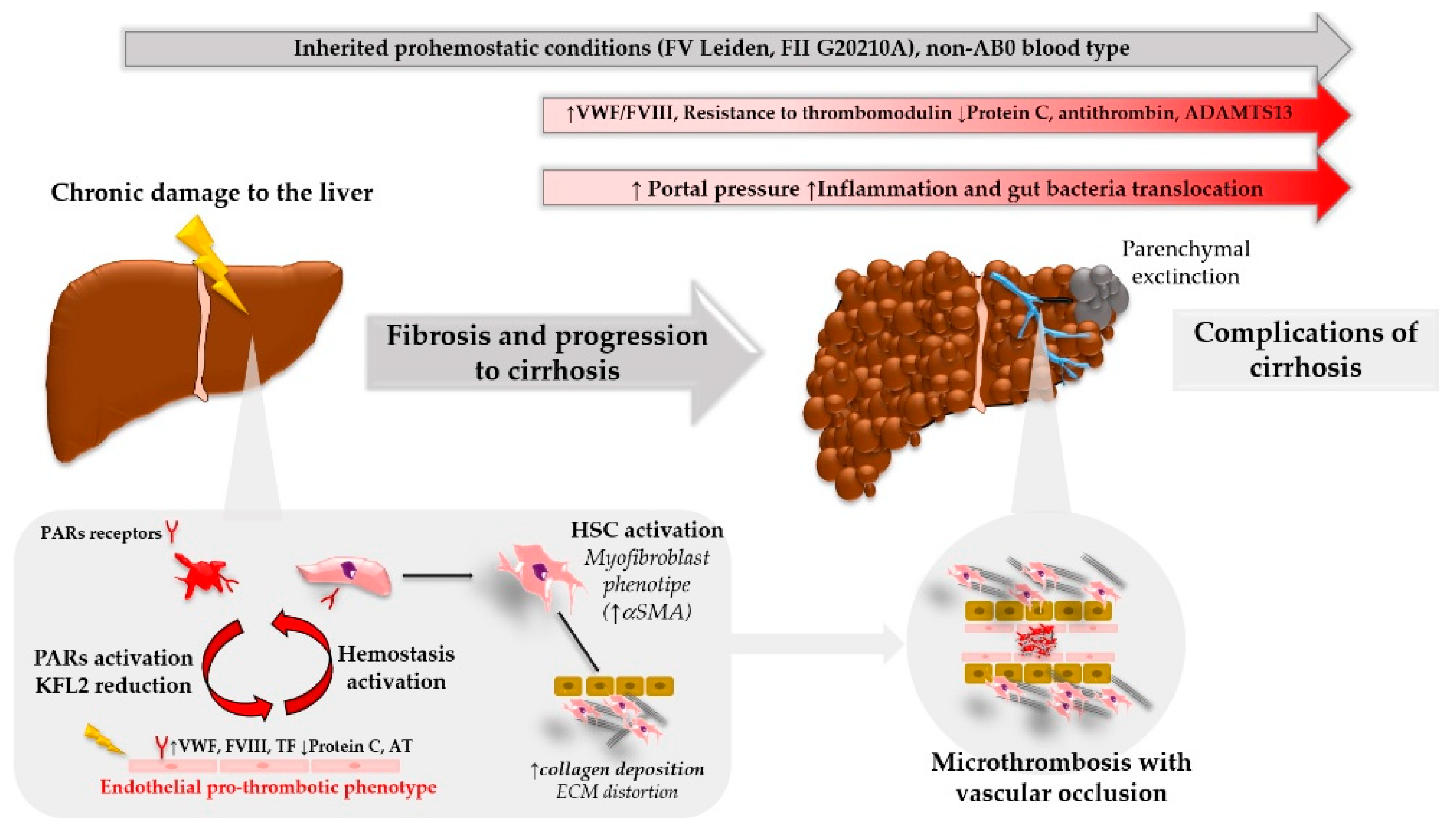
Patients with liver disease often have blood results that give an appearance of a significant bleeding risk
Mar 12, 2021
Dr. Rajesh Bollam
Navigating Uncertain Times in Muscle-Invasive and Advanced Bladder Cancer
Mar 12, 2021
Dr. Rajesh Bollam
Lenvatinib plus pembrolizumab
Mar 12, 2021
Dr. Rajesh Bollam
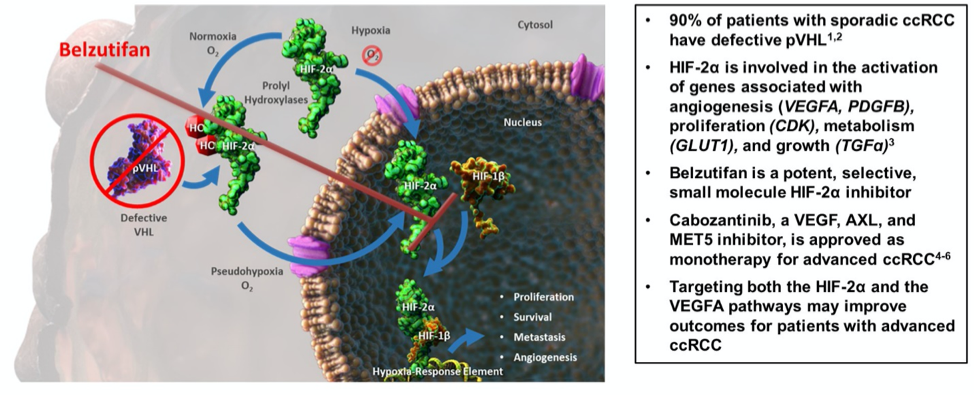
From bench to bedside, another practice-changing treatment is on the road!
Mar 12, 2021
Dr. Rajesh Bollam

ASH_hematology VTE guidelines in patients with cancer
Mar 12, 2021
Dr. Rajesh Bollam
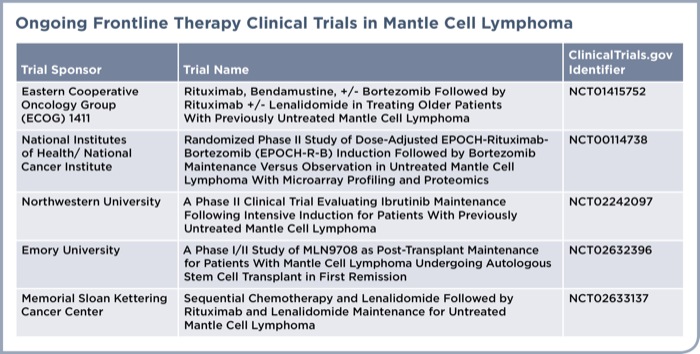
How I Rx Newly Diagnosed Mantle Cell Lymphoma
Mar 12, 2021
Dr. Rajesh Bollam
Ipilumumab plus pembrolizumab vs pembrolizumab alone in pdL1 more than 50 percentage Which is better
Mar 12, 2021
Dr. Rajesh Bollam
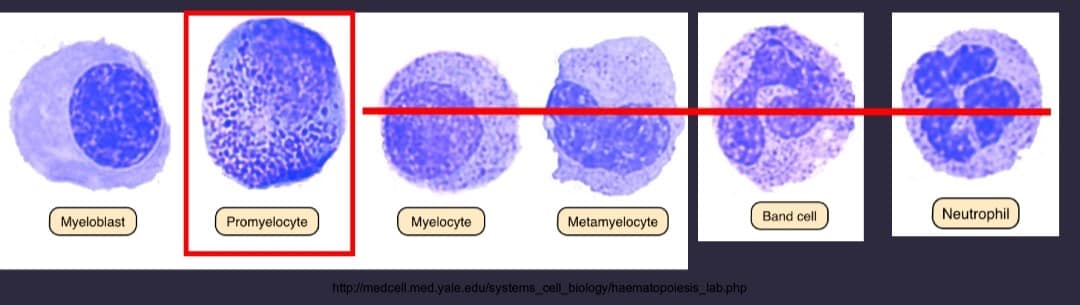
APML is medical emergency
Mar 11, 2021
Dr. Rajesh Bollam
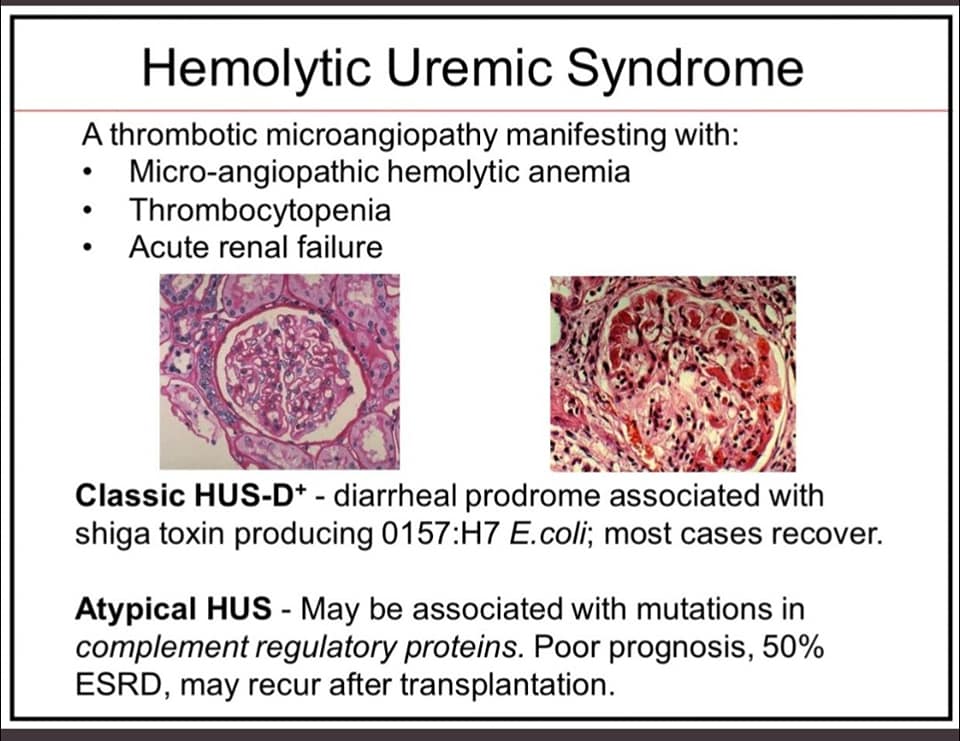
aHUS is a disease of excessive activation of the alternative complement pathway (ACP)
Mar 11, 2021
Dr. Rajesh Bollam
imp. point to reiterate
Mar 11, 2021
Dr. Rajesh Bollam
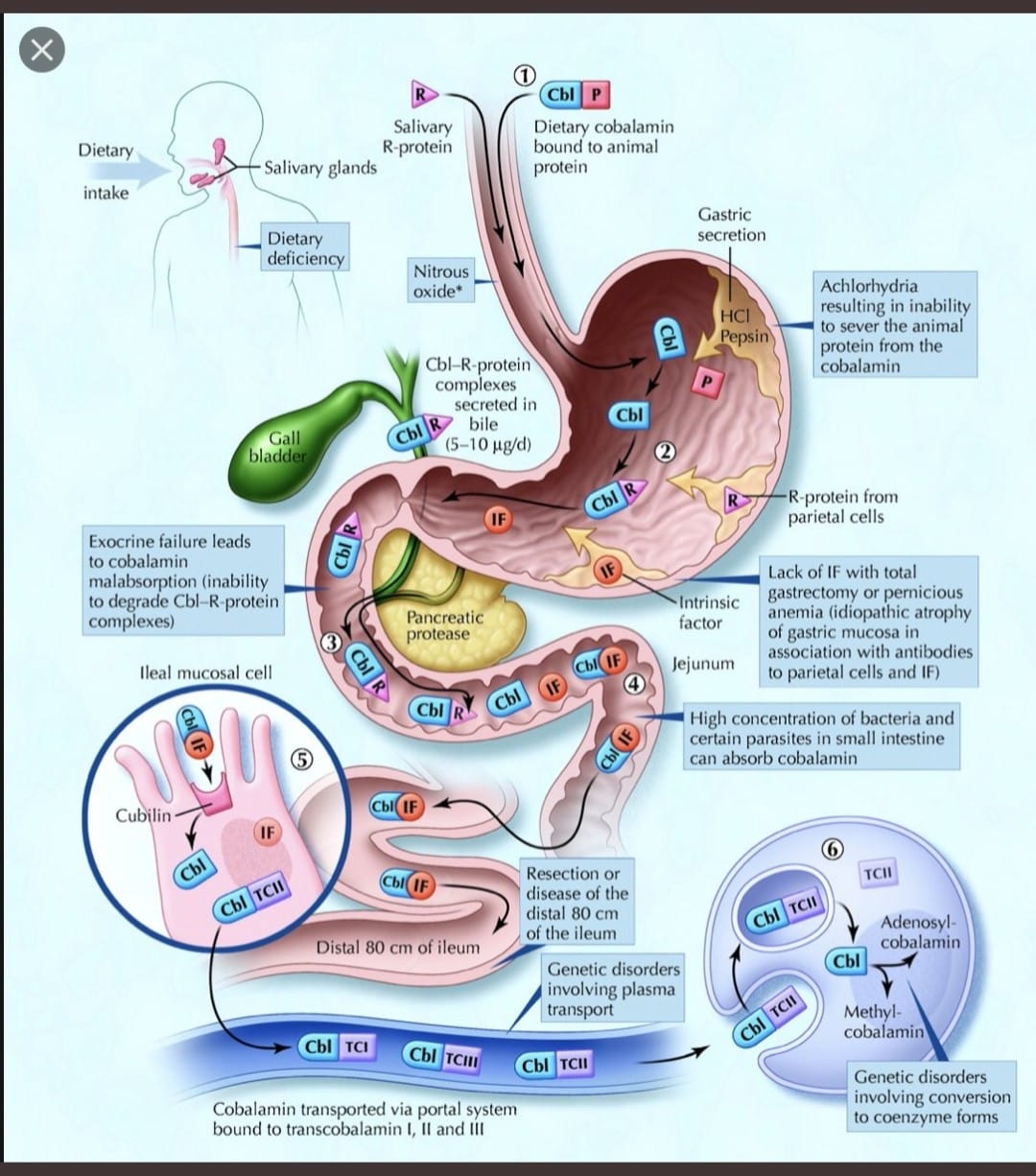
Understand B12 Absorption to Learn B12 Def
Mar 11, 2021
Dr. Rajesh Bollam
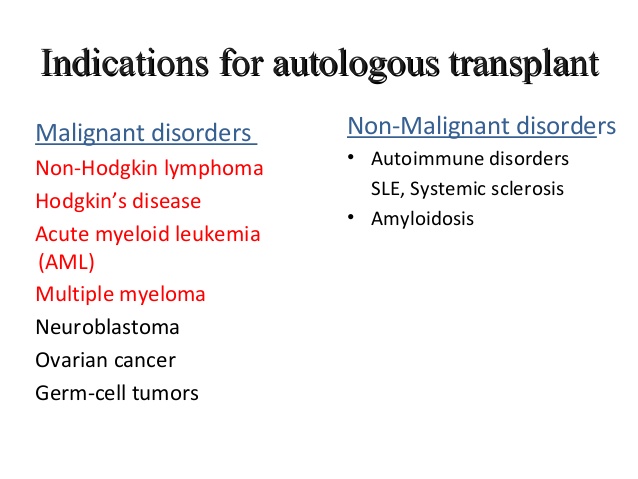
Indications for auto-transplant - for the oncology fellows
Mar 09, 2021
Dr. Rajesh Bollam
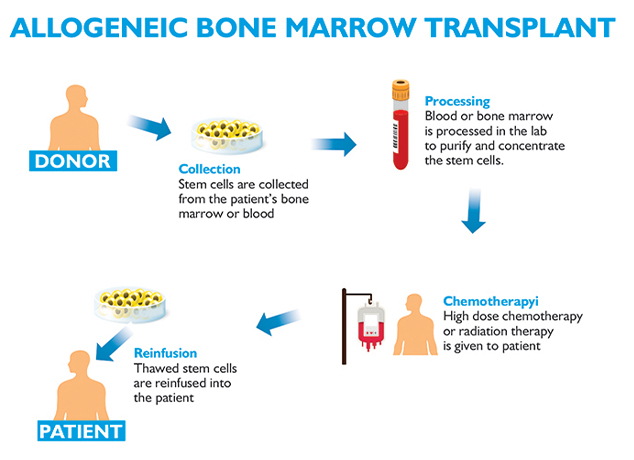
Allogeneic bone marrow transplant is the curative treatment for few relapsed leukemias and Lymphoma
Mar 09, 2021
Dr. Rajesh Bollam
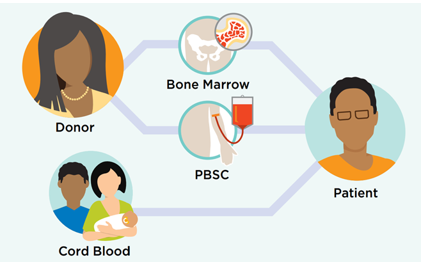
Allo BMT Basics
Mar 09, 2021
Dr. Rajesh Bollam
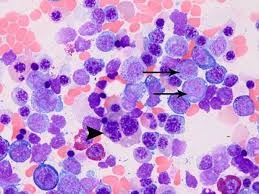
Myeloid HemePath Pearls
Mar 09, 2021
Dr. Rajesh Bollam
Myeloid HemePath Pearls
Mar 09, 2021
Dr. Rajesh Bollam
Amyloidosis month
Mar 03, 2021
Dr. Rajesh Bollam
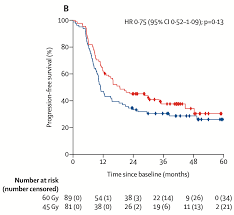
Full publication of randomized Scandinavian dose escalation trial for LS SCLC
Mar 03, 2021
Dr. Rajesh Bollam
Hemophilia
Mar 03, 2021
Dr. Rajesh Bollam

Rituximab Maintenance for Follicular lymphoma
Mar 03, 2021
Dr. Rajesh Bollam
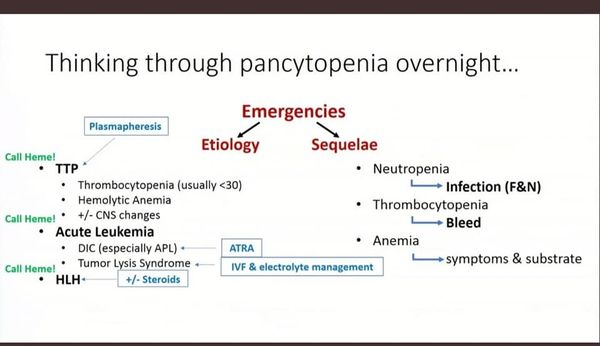
PANCYTOPENIA
Feb 23, 2021
Dr. Rajesh Bollam
WHAT IS THE MAIN CAUSE OF LYMPHOMA?
Feb 18, 2021
Dr. Rajesh Bollam
Add a comment